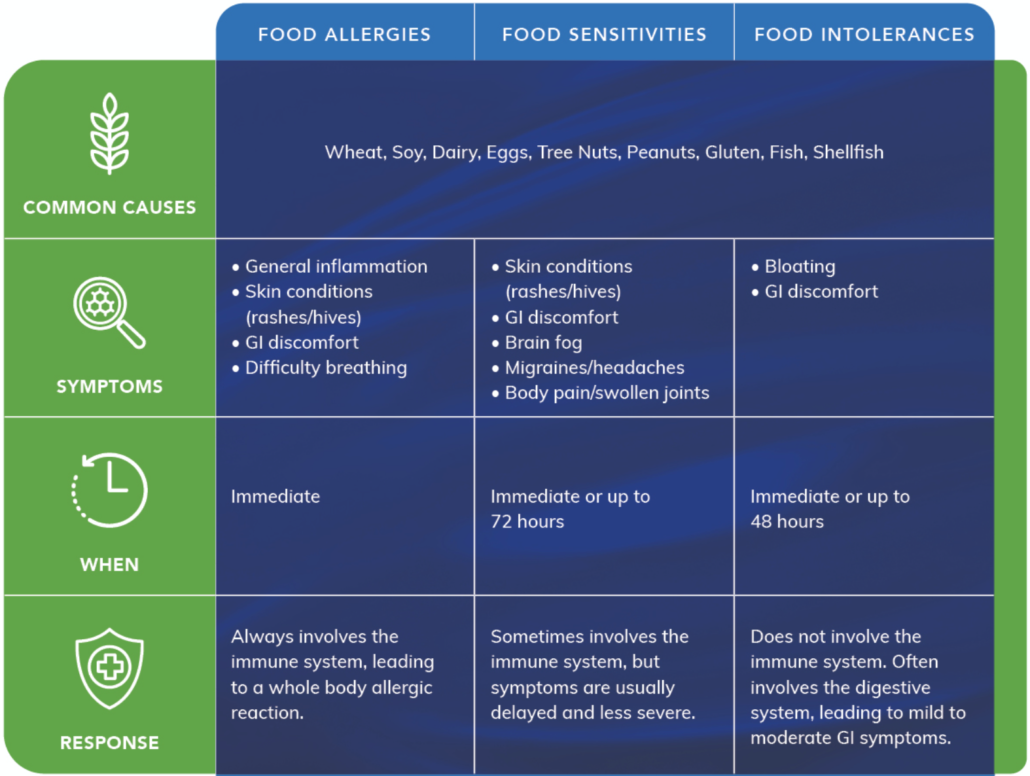
Is there a link between the food you eat and the way you feel? If you’ve ever wondered this, you aren’t alone. People are increasingly aware that even general discomforts like low energy or itchy skin may connect to your diet. Food sensitivities, food allergies, and food intolerances are all related to what you eat, but the underlying reasons why they happen differ significantly.

If you think you are reacting poorly to something you are eating, it’s helpful to understand the difference between these three, so you can make the necessary changes to feel better fast.
What is a food allergy?
The biggest reason food allergies are different from sensitivities or intolerances is how your immune system responds. Food allergies occur when antibodies (IgE antibodies) trigger the body to release molecules that drive inflammation and cause accompanying symptoms. These responses usually happen immediately after exposure to the food.
Food allergies can be life-threatening for some people because the immune system has flagged a harmless ingredient as a significant danger. The most common food allergies include:
- Peanuts
- Tree nuts
- Wheat
- Eggs
- Shellfish
- Fish
- Soy
- Cow’s milk
Reactions to food are also significantly on the rise globally. Research suggests that allergies to foods like peanuts have doubled in the United Kingdom or tripled in the United States, and similar increases were also seen in overall food allergies for children in China and India.
Cow’s milk and egg are consistently the most prevalent food allergies in children globally. Still, the prevalence of allergies can vary depending on geography and regional food patterns. 5 For example, chickpeas are a top food allergen in India, while buckwheat is an anaphylactic trigger for children in South Korea and Japan, reflecting commonly eaten foods in these countries. 5
Symptoms of food allergies
Food allergy symptoms depend on the location of the immune cells involved. They can include skin reactions like hives or rashes, GI discomfort with cramping or diarrhea, or swelling and difficulty breathing. The most severe reaction is anaphylaxis, a life-threatening response to an allergen.
How are food allergies diagnosed?
Generally, food allergies are diagnosed by a health care practitioner specializing in allergy and immunology. Testing can include a blood or skin prick test with appropriate interpretation by the physician. While some childhood allergies reduce with age, for most people, once diagnosed, that ingredient has to be avoided forever, and even small amounts can cause a response. 1
What causes food allergies?
The underlying reasons for food allergies are complex, and scientists believe they are likely related to a combination of genetics and environment. This means that you may be predisposed to develop an allergy if you have a family member with food allergies, but exposures or habits can increase the risk. Aside from gender and genetics, some of the possible risk factors include:
- Low vitamin D status
- C-section delivery
- Age of first food introduction
Are food sensitivities the same as food allergies?
The short answer is no. Food sensitivities may involve the immune system, but the pathway is different than food allergies. They also don’t cause anaphylaxis.
However, just because they aren’t life-threatening doesn’t mean that sensitivities don’t significantly impact your health. Like allergies, they can activate your white blood cells to release pro-inflammatory mediators that lead to symptoms (but don’t involve IgE antibodies).
Food sensitivities can occur soon after ingesting the ingredient, but you might not have a response for up to 72 hours later. This is known as delayed hypersensitivity.
Are food sensitivities as common as food allergies?
Tracking the prevalence of food sensitivities isn’t easy because there isn’t a well-regarded diagnostic tool (as you will learn below). There are common sensitivities such as non-celiac gluten sensitivity (NCGS), but responses can also happen with chemicals or additives in the food itself, including chemicals like food coloring or sulfites or naturally occurring compounds like caffeine in chocolate.
What are the symptoms of food sensitivities?
Because the inflammatory mediators travel throughout your body, they can affect many different body systems. Symptoms of food sensitivities can range from mild to severe and can include:
- GI-related such as nausea, constipation, vomiting, diarrhea, bloating, or cramping
- Brain fog
- Skin conditions and rashes
- Migraines or headaches
- Body pain and swollen joints
How are food sensitivities diagnosed?
As mentioned, diagnosing food sensitivities can be tricky and is usually based on a process of elimination. For some time, food sensitivities were not well recognized in the medical field, but because of rising cases such as NCGS, they are increasingly recognized. However, they are still not as well understood as food allergies.
Standard food allergy tests won’t show food sensitivities because they involve completely different parts of the immune system. While there are several food sensitivity tests available, most are not well validated.
As a result, food sensitivity tests can act as a starting point, but elimination diets are the accepted gold standard. And since food sensitivities can be so delayed or symptoms are easily chalked up to other health conditions, working with a healthcare practitioner specializing in food sensitivities can help you narrow down the problematic ingredient.
What causes food sensitivities?
The reasons for food sensitivities are not entirely understood, though many experts suggest that a likely cause is related to gut dysbiosis, an imbalance of your commensal gut bacteria. An unhealthy gut can also damage your intestinal lining. When the gut lining is compromised, it can allow unwanted food proteins and other molecules into circulation, causing an immune response. 22
It’s common to have more than one food sensitivity, unlike allergies or intolerances that are often specific to one or two foods. Sensitivities can also change over time. Unlike allergies which remain constant (aside from children who grow out of them), addressing the reason you have the sensitivities, such as inflammation from dysbiosis, can improve the sensitivity over time for some people.
What are food intolerances?
Sometimes food intolerances are incorrectly labeled food sensitivities, but they aren’t the same. While symptoms can be similar, intolerances are different because they don’t involve the immune system at all. Instead, food intolerances occur in the gut due to functional digestive issues that cause difficulty digesting specific foods.
What are common food intolerances?
The most common food intolerance is lactose intolerance. This happens when you lack the enzyme lactase that breaks down lactose, a sugar found in dairy products. Globally it’s estimated that 68% of the world’s population has some form of lactose malabsorption.
Another common intolerance is related to foods containing FODMAPs. FODMAPs is an acronym that stands for fermentable oligosaccharides, disaccharides, monosaccharides, and polyols, a group of short-chain carbohydrates. People with FODMAP intolerance have a difficult time digesting these foods.
What are the symptoms of food intolerances?
Because intolerances are related to issues digesting specific foods, symptoms of intolerances tend to stay in the GI tract and include:
- Bloating
- Constipation
- Pain
- Diarrhea
- Gas
How are food intolerances diagnosed?
Generally, food intolerances are also diagnosed by an elimination diet with the suspected food. For example, with lactose intolerance, simply removing dairy resolves symptoms. There is a test for lactose intolerance, but many physicians just have their patients remove dairy to avoid a more invasive procedure.
Support your health by addressing your food-related symptoms
If you suspect there’s a relationship between what you eat and how you feel, getting to the root cause is vital for feeling like yourself again. Allergies are the most serious of the three, but food sensitivities or intolerance can still significantly impair your quality of life. Once you figure out what food your body is reacting to, it’s essential to avoid that ingredient, no matter the underlying reason. Even trace amounts can impact sensitive people, so it’s critical to know how to check all your food labels—including your supplements—to ensure you are completely avoiding them. Whether a food allergy, food intolerance, or food sensitivity, working with the appropriate healthcare practitioner to guide you through testing and elimination is especially helpful for supporting your long-term health.
- “Food Allergy.” Text. National Library of Medicine. Accessed September 24, 2021. https://medlineplus.gov/foodallergy.html.
- Seth, Divya, Pavadee Poowutikul, Milind Pansare, and Deepak Kamat. “Food Allergy: A Review.” Pediatric Annals 49, no. 1 (January 1, 2020): e50–58. https://doi.org/10.3928/19382359-20191206-01.
- Loh, Wenyin, and Mimi L. K. Tang. “The Epidemiology of Food Allergy in the Global Context.” International Journal of Environmental Research and Public Health 15, no. 9 (September 2018): 2043. https://doi.org/10.3390/ijerph15092043.
- Sicherer, Scott H., and Hugh A. Sampson. “Food Allergy: Epidemiology, Pathogenesis, Diagnosis, and Treatment.” The Journal of Allergy and Clinical Immunology 133, no. 2 (February 2014): 291–307; quiz 308. https://doi.org/10.1016/j.jaci.2013.11.020.
- Jm, Devdas, Mckie C, Fox At, and Ratageri Vh. “Food Allergy in Children: An Overview.” Indian Journal of Pediatrics 85, no. 5 (May 2018). https://doi.org/10.1007/s12098-017-2535-6.
- Anaphylaxis Campaign. “Signs and Symptoms.” Accessed September 24, 2021. https://www.anaphylaxis.org.uk/hcp/what-is-anaphylaxis/signs-and-symptoms/.
- Sicherer, Scott H., and Hugh A. Sampson. “Food Allergy: A Review and Update on Epidemiology, Pathogenesis, Diagnosis, Prevention, and Management.” Journal of Allergy and Clinical Immunology 141, no. 1 (January 1, 2018): 41–58. https://doi.org/10.1016/j.jaci.2017.11.003.
- Poole, Ashlyn, Yong Song, Helen Brown, Prue H. Hart, and Guicheng (Brad) Zhang. “Cellular and Molecular Mechanisms of Vitamin D in Food Allergy.” Journal of Cellular and Molecular Medicine 22, no. 7 (July 2018): 3270–77. https://doi.org/10.1111/jcmm.13607.
- Papathoma, Evangelia, Maria Triga, Sotirios Fouzas, and Gabriel Dimitriou. “Cesarean Section Delivery and Development of Food Allergy and Atopic Dermatitis in Early Childhood.” Pediatric Allergy and Immunology: Official Publication of the European Society of Pediatric Allergy and Immunology 27, no. 4 (June 2016): 419–24. https://doi.org/10.1111/pai.12552.
- Perkin, Michael R., Kirsty Logan, Henry T. Bahnson, Tom Marrs, Suzana Radulovic, Joanna Craven, Carsten Flohr, et al. “Efficacy of the Enquiring About Tolerance (EAT) Study among Infants at High Risk of Developing Food Allergy.” The Journal of Allergy and Clinical Immunology 144, no. 6 (December 2019): 1606-1614.e2. https://doi.org/10.1016/j.jaci.2019.06.045.
- Abdulkhaleq, L. A., M. A. Assi, Rasedee Abdullah, M. Zamri-Saad, Y. H. Taufiq-Yap, and M. N. M. Hezmee. “The Crucial Roles of Inflammatory Mediators in Inflammation: A Review.” Veterinary World 11, no. 5 (May 2018): 627–35. https://doi.org/10.14202/vetworld.2018.627-635.
- Marshall, Jean S., Richard Warrington, Wade Watson, and Harold L. Kim. “An Introduction to Immunology and Immunopathology.” Allergy, Asthma, and Clinical Immunology: Official Journal of the Canadian Society of Allergy and Clinical Immunology 14, no. Suppl 2 (2018): 49. https://doi.org/10.1186/s13223-018-0278-1.
- Leonard, Maureen M., Anna Sapone, Carlo Catassi, and Alessio Fasano. “Celiac Disease and Nonceliac Gluten Sensitivity: A Review.” JAMA 318, no. 7 (August 15, 2017): 647–56. https://doi.org/10.1001/jama.2017.9730.
- Mansueto, Pasquale, Aurelio Seidita, Alberto D’Alcamo, and Antonio Carroccio. “Non-Celiac Gluten Sensitivity: Literature Review.” Journal of the American College of Nutrition 33, no. 1 (2014): 39–54. https://doi.org/10.1080/07315724.2014.869996.
- Croall, Iain D., Nigel Hoggard, Imran Aziz, Marios Hadjivassiliou, and David S. Sanders. “Brain Fog and Non-Coeliac Gluten Sensitivity: Proof of Concept Brain MRI Pilot Study.” PLoS ONE 15, no. 8 (2020). https://doi.org/10.1371/journal.pone.0238283.
- Palmo, Emanuela di, Marcella Gallucci, Francesca Cipriani, Luca Bertelli, Arianna Giannetti, and Giampaolo Ricci. “Asthma and Food Allergy: Which Risks?” Medicina 55, no. 9 (August 21, 2019): 509. https://doi.org/10.3390/medicina55090509.
- Özön, Akçay Övünç, Ömer Karadaş, and Aynur Özge. “Efficacy of Diet Restriction on Migraines.” Archives of Neuropsychiatry 55, no. 3 (September 20, 2016): 233–37. https://doi.org/10.5152/npa.2016.15961.
- Raoof, Ramin, Hanneke L D M Willemen, and Niels Eijkelkamp. “Divergent Roles of Immune Cells and Their Mediators in Pain.” Rheumatology (Oxford, England) 57, no. 3 (March 2018): 429–40. https://doi.org/10.1093/rheumatology/kex308.
- Barbaro, Maria Raffaella, Cesare Cremon, Vincenzo Stanghellini, and Giovanni Barbara. “Recent Advances in Understanding Non-Celiac Gluten Sensitivity.” F1000Research 7 (2018). https://doi.org/10.12688/f1000research.15849.1.
- Tuck, Caroline J., Jessica R. Biesiekierski, Peter Schmid-Grendelmeier, and Daniel Pohl. “Food Intolerances.” Nutrients 11, no. 7 (July 22, 2019): E1684. https://doi.org/10.3390/nu11071684.
- Vandenplas, Y. “Debates in Allergy Medicine: Food Intolerance Does Exist.” The World Allergy Organization Journal 8 (December 14, 2015): 36. https://doi.org/10.1186/s40413-015-0087-7.
- Caminero, Alberto, Marlies Meisel, Bana Jabri, and Elena F. Verdu. “Mechanisms by Which Gut Microorganisms Influence Food Sensitivities.” Nature Reviews Gastroenterology & Hepatology 16, no. 1 (January 2019): 7–18. https://doi.org/10.1038/s41575-018-0064-z.
- Zopf, Yurdagül, Eckhart G. Hahn, Martin Raithel, Hanns-Wolf Baenkler, and Andrea Silbermann. “The Differential Diagnosis of Food Intolerance.” Deutsches Ärzteblatt International 106, no. 21 (May 2009): 359–70. https://doi.org/10.3238/arztebl.2009.0359.
- Storhaug, Christian Løvold, Svein Kjetil Fosse, and Lars T. Fadnes. “Country, Regional, and Global Estimates for Lactose Malabsorption in Adults: A Systematic Review and Meta-Analysis.” The Lancet. Gastroenterology & Hepatology 2, no. 10 (October 2017): 738–46. https://doi.org/10.1016/S2468-1253(17)30154-1.
- Gibson, Peter R., and Susan J. Shepherd. “Evidence-Based Dietary Management of Functional Gastrointestinal Symptoms: The FODMAP Approach.” Journal of Gastroenterology and Hepatology 25, no. 2 (February 2010): 252–58. https://doi.org/10.1111/j.1440-1746.2009.06149.x.
- Savaiano, Dennis A., Andrew J. Ritter, Todd R. Klaenhammer, Gareth M. James, Amy T. Longcore, Justin R. Chandler, W. Allan Walker, and Howard L. Foyt. “Improving Lactose Digestion and Symptoms of Lactose Intolerance with a Novel Galacto-Oligosaccharide (RP-G28): A Randomized, Double-Blind Clinical Trial.” Nutrition Journal 12 (December 13, 2013): 160. https://doi.org/10.1186/1475-2891-12-160.
Share:
Related Posts

TUDCA vs. Milk Thistle: Which One Supports Your Liver Best?
Written by Ashley Palmer & Pooja Mahtani | 2025 Key Takeaways: TUDCA is a bile acid that enhances bile flow, reduces liver inflammation, and supports

14 Common Questions About PectaSol Modified Citrus Pectin
Written by ecoNugenics An increased interest in natural therapies to treat the body has led to exciting research into a variety of supplements. One common

Benefits of Creatine in Perimenopause and Menopause
Written by Maura MacDonald, MS, RD, CSSD | 2025 As we age, the notion is that we will inevitably become weaker. Not as mobile as

Goodbye Pie Chart, Hello Phase 1 Sliders
Written by Allison Smith, ND | 2025 As we usher in a new era of DUTCH testing which leaves behind the concept of the three-way

Introducing the DUTCH Dozen
Written by Kelly Ruef, ND | 2025 Hormone testing can be complex, which is why Precision Analytical developed the DUTCH Dozen, an interpretive framework that

