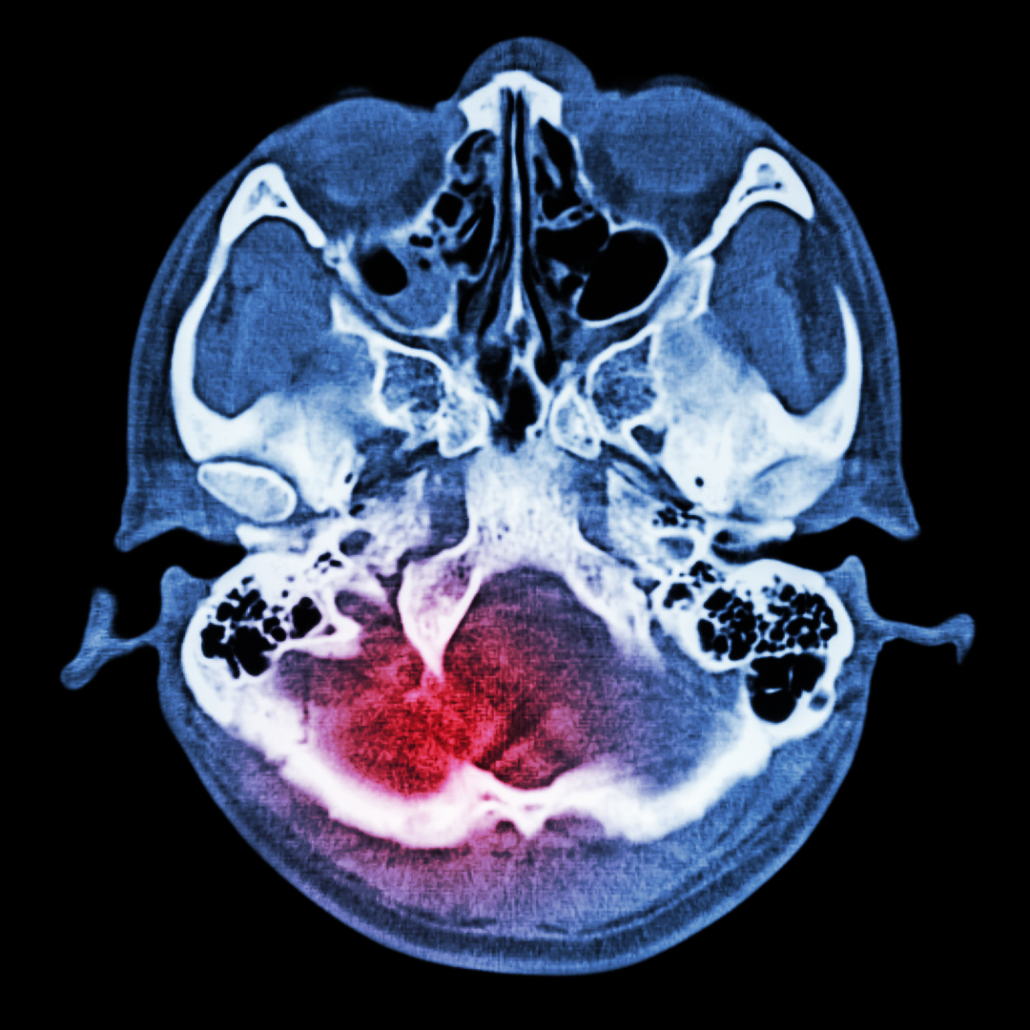
Systemic inflammation in the body can trigger inflammation in the brain. Previously it was thought that our blood brain barrier protected the brain from insult. Now we understand that inflammatory mediators can damage cell membranes leading to a leaky blood brain barrier. In medicine, the concept of an intestinal barrier with hyper permeability is generally accepted. Now we have a blood brain barrier with increased permeability.
Neuroinflammation is well known in diseases such as Alzheimer’s and Parkinson’s. It is also a component of diseases in children such as autism and the common disease of depression. Many chronic systemic diseases have systemic inflammation such as cystic fibrosis which results in mood issues from neuroinflammation. Even when you have an acute infection such as influenza you can get neuroinflammation.



Immune Pathology in the Brain
The immune system in the brain is meant to work acutely as a normal host-defense mechanism to restore normal structure and function of the brain after an insult such an injury or infection. The problem is when this system is continuously activated. In the nervous system, there are two major glial cells involved in the immune system.
First are the astrocytes which are the most abundant glial cells occupying 25% of cerebral volume. Their functions are multiple and include: promoting formation of the neuronal synapses, forming and maintaining the blood brain barrier, neurotransmission by being part of the neuronal synapse, metabolic regulation, ion balance maintenance, and development of the nervous system. Astrocytes are also involved in glutamate metabolism. These cells help eliminate excess glutamate which is critical in preventing excitotoxicity. Excitotoxicity can worsen neuroinflammation.
Microglia are the other type of glial cell involved in neuroinflammation and exist primarily in the Hippocampus and the Substantia Nigra. They are the first line of innate immune defense in the brain. Initial activation of microglia is neuroprotective but repeated activation is pro-inflammatory. Microglia have multiple functions in a similar manner as the astrocytes. They play a role in embryonic development, secrete growth factors, contribute to maturation, regeneration, and plasticity of neurons and are involved in synaptic pruning.
Usually these cells are in a resting or inactivated state. When they are activated, they are the primary source of pro-inflammatory factors in the brain. Uncontrolled activation of microglia leads to release of inflammatory cytokines (TNF-alpha, IL-6, IL-1B), nitric oxide, prostaglandin E2, and reactive oxygen and nitrogen species. Once activated microglia become macrophage cells where they engulf damaged cells along with intact neighboring neurons. Chronic neuroinflammation leads to neurodegeneration and ultimately cell death. If this was not frightening enough, the inflammatory compounds that the activated astroglia and microglia release disrupt the blood brain barrier.
The brain uses a large amount of energy compared to other organs in the body. Since mitochondria are responsible for cellular energy, they need to function well to create enough energy. Unfortunately, mitochondria are sensitive to oxidative stress. Increasing inflammation in the brain leads to increased oxidative stress and damage to the mitochondria. Mitochondria dysfunction is involved in activated neuroinflammation associated with eurodegenerative diseases such as Alzheimer’s and Parkinson’s among others1.
Systemic Inflammation leads to Neuroinflammation
Encephalitis or inflammation of the brain was once thought to be only from infections entering the brain. Systemic infections and inflammation can cause microglial activation leading to brain inflammation2. It appears that peripheral cytokines can enter the brain and activate the microglia and the astrocytes creating neuroinflammation3,4.
In effect, peripheral cytokines lead to microglial release of neural cytokines. If this process continues, a destructive cycle is created leading to cell destruction and damage to the blood brain barrier which can further increase the inflammatory mediators entering the nervous system.
Gut-brain Inflammation Connection
Systemic inflammation can reach the central nervous system through the blood to induce activation of the immune glial cells. The gastrointestinal tract is another route of connection. The gastrointestinal system is connected to the brain in the gut-brain connection where there is a bidirectional communication system5. The brain is involved in regulating the immune system and the intestine which is a large part of the immune system.
An example is the pathogen Helicobacter Pylori found in the stomach that can induce both humoral and cellular immune responses that cross-react with neural tissue and may be involved in Multiple Sclerosis6. Chronic irritable bowel syndrome often associated with dysbiosis or an increase in pathogenic bacteria in the microbiome can lead to an increase in systemic inflammatory cytokines and LPS causing neuroinflammation5 . Dysbiosis leading to dysfunctional bidirectional gut-brain axis promotes neuroinflammation.
Triggers for neuroinflammation
Considering that systemic inflammation and gastrointestinal inflammation can lead to neuroinflammation, the number of potential causes is daunting. The causes can be grouped into categories. Systemic infections that can have neuroinflammation include diseases such as Lyme disease7 , HHV6, measles, varicella, HIV, and West Nile Virus not to mention the specific encephalitis viruses and bacteria such as Neisseria meningococcus. Pathogenic organisms in the intestines such as H. Pylori can trigger inflammation that proceeds to the nervous system8.
Multiple environmental chemicals can cause neuroinflammation. Heavy metals such as mercury and lead are known neurotoxins. Air pollution and the chemicals in passive smoke exposure can increase risk of neuroinflammation9. Traumatic brain injury releases pro-inflammatory cytokines such as IL-1B that activate microglia. Autoimmune reactions from infections such as strep bacteria can lead to neuroinflammation. Finally, the inevitable aging increases risk of neuroinflammation by causing an imbalance of anti-inflammatory and pro-inflammatory cytokines which increase the number of activated microglia.


Diseases with Neuroinflammation:
The list of neurodegenerative diseases associated with neuroinflammation is well known. Alzheimer’s disease is the most common cause of dementia in people over 60 years old. The pathology involves an accumulation of intracellular neurofibrillary tangles and extracellular amyloid plaques leading to neuroinflammation and finally cell destruction10. Parkinson’s has a progressive loss of dopaminergic neurons primarily in the Substantia Nigra11. Amyotrophic lateral sclerosis and Multiple Sclerosis are also chronic degenerative diseases associated with neuroinflammation. Mental health issues such as depression and bipolar disease are associated with underlying inflammation. How we treat these mental health issues needs to shift its focus to incorporate anti-inflammatory treatment.
Children unfortunately are not immune to neuroinflammation. Autism and ADHD are both diseases with neuroinflammation as the underlying cellular mechanism. Children with autism have been shown to have microglial and astrocytic activation along with pro-inflammatory cytokines in both the nervous system and systemically12,13. Chronic microglial activation causes cell loss and reduced connectivity which are both found in brains of those with autism. The greater the cell loss and connectivity issues, the worse the symptoms of autism14. When the pathology of neuroinflammation in Alzheimer’s is compared to autism, the activation of microglia and astrocytes with subsequent release of pro-inflammatory cytokines is similar12. If we have children with neuroinflammation like adults with neurodegenerative disease, we have serious problems ahead for our society.
Hope through Natural Treatments:
Although there has been great progress in understanding neuroinflammation, our options for treatments with traditional medicines have been limited. Due to our decreased ability to find effective medicines, natural treatments have become increasingly important.
When discussing inflammation, nutrition is always a primary starting point. A high sugar, highly processed diet promotes inflammation. A plant diet high in fruits and vegetables with their active phytonutrients is anti-inflammatory. Incorporating omega 3 fats through food or supplements are critical anti-inflammatory nutrients15. Vitamin E in the form of tocotrienols and full spectrum vitamin E incorporating the gamma components are good anti-oxidants along with vitamin C15. Magnesium and zinc are also crucial minerals to combat neuroinflammation15. General immune and digestive support with probiotics is also beneficial.
Many of the phytonutrients when isolated from plants have been found to be very effective in moderating neuroinflammation16. Curcumin, the active ingredient in the herb Turmeric has shown effectiveness against neuroinflammation17,18. Research has shown Curcumin to be effective at down regulating many pro-inflammatory cytokines which may explain part of its effectiveness. The primary problem with Curcumin is its poor bioavailability which can be bypassed using a form with increased absorbability. Resveratrol is another plant component with research showing its anti-inflammatory effects both systemically and in the nervous system19. In animal models, resveratrol decreased inflammatory markers along with symptomatic behavior20,21. Flavonoids such as luteolin can be useful in treating neuroinflammation. EGCG, a component of green and black tea has neuroprotective properties.
Since mitochondrial dysfunction is involved in neuroinflammation, repair and support of this cellular component is critical. The mitochondria have a lipid membrane similar to the cell membrane that is damaged by oxidative stress. Repair of this fatty membrane with targeted phospholipids is important. Supporting the mitochondria with nutrients such as CoQ10, Carnitine, alpha-lipoic acid, and B-vitamins is crucial22. A compound, molecular hydrogen or hydrogen water is a new treatment that targets neuroinflammation. It is a covalently bound stable form of hydrogen with strong fat solubility making it easy to cross the blood brain barrier. Once inside the brain it neutralizes the strong free hydroxy radical without harming the free radicals needed for normal metabolism23,24. Through cell signaling it decreases pro-inflammatory cytokines23. It promotes mitochondrial ATP function. Finally, it has additional anti-oxidant capabilities by activating the Nrf2 cascade increasing anti-oxidant enzymes including glutathione peroxidase, catalase, and superoxide dismutase (SOD).
Another advantage of molecular hydrogen is ease of use. It can be dissolved and then consumed in water. The safety profile is excellent25. Awareness of the compound was brought about through a study by Ohta in 2007 showing its anti-oxidant and anti-inflammatory mechanisms of action23.
One of the most important properties of molecular hydrogen is its ability to protect against neuroinflammation. Many of our treatments target ongoing inflammation but molecular hydrogen can work pro-actively to prevent neuroinflammation. Research has studied this concept of neuroprotection in studies with traumatic brain injury, surgery, and stroke animal models 26,27,28.

Summary
Neuroinflammation or inflammation in the nervous system is gaining recognition as a significant factor in many chronic diseases. Systemic and gastrointestinal inflammation can cause or exacerbate neuroinflammation. Awareness of the connection between the brain and the body through the gut-brain neural connections and the systemic immune system is critical for our understanding and treatment of this issue
- Onyango IG. Et al. Mitochondria in the pathophysiology of Alzheimer’s and Parkinson’s diseases. Front Biosci (Landmark Ed). 2017 Jan1; 22:854‐872.
- Teeling JL. Et al. systemic infection and inflammation in acute CNS injury and chronic neurodegeneration: Underlying mechanisms. Neuroscience. 2009. 158, 1062‐1073.
- Banks WA. Et al. Blood to brain transport of interleukin links the immune and central nervous systems. Life Sci. 1991. 48. L117‐L121.
- Gutierrez EG. Et al. Murine tumor necrosisfactor alpha istransported from blood to brain in the mouse. J. Neuroimmunol. 47, 169‐176.
- Daulatzai, MA. Chronic functional bowel syndrome enhances gut‐brain axis dysfunction, neuroinflammation, cognitive impairment and vulnerability to dementia. Neurochemical Research. 2014 April Vol 39(4)
- Deretzi G. Et al. Gastrointestinal immune system and brain dialogue implicated in neuroinflammatory and neurodegenerative diseases. Current Molecular Medicine. 2011
Nov. Vol 11(8). - Pietikainen A. Et al. Cerebrospinal fluid cytokines in Lyme neuroborreliosis. J. Neuroinflammation. 2016 Oct 18: 13(1).
- Budzyniski J. Et al. Brain‐gut axis in the pathogenesis of Helicobacter Pylori infection. World J Gastroenterol. 2014 May 14:20(18).
- Black ML. Et al. Air pollution: mechanisms of neuroinflammation and central nervous system disease. Trends in Neurosciences. 2009 Sept Vol 32(9).
- MoralesI. Et al. Neuroinflammation in the pathogenesis of Alzheimer’s disease: A rational framework forthe search of novel therapeutic approaches. Front Cell Neurosci. 2014 April 22;8‐112.
- Vasant MS. Et al. Cellular and molecular mediators of neuroinflammation in the pathogenesis of Parkinson’s disease. Hindawi Pub. Corporation. Mediators of
Inflammation 2013. - Vargas DL, Nascimbene C, Krishnan C, Zimmerman AW, Pardo CA. Neuroglial activation and neuroinflammation in the brain of patients with autism. Ann Neurol. 2005
Jan;57(1):67‐81. - Li X. Et al. Elevated immune response in the brain of autistic patients. J Neuroimmunol 2009 207:111‐116.
- Kern JK. Et al. Relevance of Neuroinflammation and Encephalitis in autism. Frontiers in Cellular Neuroscience. 2016 Jan.
- Vonder Haar C. Et al. vitamins and nutrients as primary treatments in experimental brain injury: Clinical implications for nutraceutical therapies. Brain Res. 2016 Jun 1:1640(Pt A:114‐29.
- Perez‐Hernandez J. Et al. A potential alternative agent for neurodegenerative diseases: Phytodrugs. Oxidative medicine and cellular longevity. 2016.
- Kim SJ. Et al. Curcumin stimulates proliferation of embryonic neural progenitor cells and neurogenesis in the adult hippocampus. J Biol Chem. 283.
- Hoppe JB. Et al. Curcumin protects organotypic hippocampal slice cultures from Abt‐a42‐induced synaptic toxicity. Toxicol In Vitro. 27.
- Lu C. Et al. Design, synthesis, and evaluation of resveratrol derivatives as AB (1‐42) aggregation inhibitors, anti‐oxidants, and neuroprotective agents. Bioorg Med Chem
Letter. 22. - Bhandari R. Et al. Resveratrol suppresses neuroinflammation in the experimental paradigm of autism spectrum disorders. Neurochem Int. 2017 Feb; 103:8‐23.
- Abraham J. Et al. Consuming a diet supplemented with resveratrol reduced infection related neuroinflammation and deficits in working memory in aged mice. Rejuvenation
Research. 2009 Dec. Vol 12(6). - D’Mello F. Et al. Cytotoxic effects of environmental toxins in human glial cells. Neurotox Res. 2017 Feb.
- Ichihara, M., et al., Beneficial biological effects and the underlying mechanisms of molecular hydrogen ‐ comprehensive review of 321 original articles. Med Gas Res. 2015.
5: p. 12. - Ohta, S., Molecular hydrogen as a preventive and therapeutic medical gas: initiation, development and potential of hydrogen medicine. Pharmacol Ther. 2014.
- Saitoh Y, et al. Biologicalsafety of neutral‐pH hydrogen‐enriched electrolyzed water upon mutagenicity, genotoxicity, and subchronic oral toxicity. Toxicology and Industrial health. 2010. 26(4):203‐216.
- Dohi, K., et al., Molecular Hydrogen in Drinking Water Protects against Neurodegenerative Changes Induced by Traumatic Brain Injury. PLoS One. 2014. 9(9): p. e108034.
- Domoki, F., et al., Hydrogen is Neuroprotective and Preserves Cerebrovascular Reactivity in Asphyxiated Newborn Pigs. Pediatric Research. 2010. 68(5): p. 387‐392.
- Eckermann, J.M., et al., Hydrogen is neuroprotective against surgically induced brain injury. Medical Gas Research. 2011. 1(1): p. 7.
Share:
Related Posts

Why Would I Test Positive To Foods On A Dietary Antigen Test That I Don’t Eat?
Written by Precision Point Diagnostics | 2025 True food allergies are when the body develops antibodies against a particular food, or a related food. Patients
Mitochondria: The Overlooked Link in the Gut-Brain Axis
Written by Dr Sarah Daglis | 2025 The gut-brain axis is well-established, but there’s more to this dynamic relationship than meets the eye. A vital

Unlocking Respiratory Resilience Through Functional Medicine
Article written by Dr Michelle Clark Naturopathic Doctor Clinical Education Manager, FxMed Published 1 September 2024 People take supplements to improve or optimize their health.

AHCC: Unlocking the Immune Intelligence of Shiitake Mycelia
Article written by Jessica Sanders BSc. (Psy), Dip Nat, Dip Med Herb Technical Projects, FxMed Published 1 September 2024 People take supplements to improve or

Life After Weight Loss Meds
Kathi Head, ND February 20, 2025 You would have to have been spending glorious hours lying on the beach on a desert island not to



